Abstract

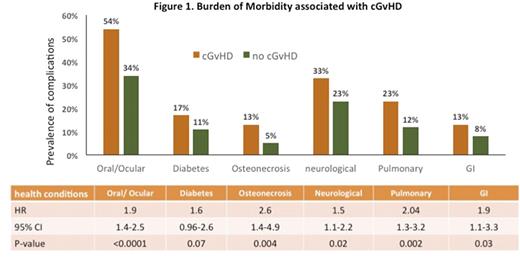
Background: Patients with cGvHD are at risk for morbidity and compromised quality of life. However, the risk of specific morbidities observed long-term in patients with cGvHD is not clearly understood. Furthermore, whether patients with cGvHD are more likely to be frail, with added vulnerability to an already compromised functional status, remains unstudied. Methods: Study participants were drawn from BMTSS - a retrospective cohort of patients who had received a BMT at City of Hope or University of Minnesota between 1974 and 1998 for a hematologic malignancies or severe aplastic anemia (SAA) and survived at least 2y post-BMT. This study included 581 allogeneic BMT recipients ≥18y of age at study participation and alive at baseline survey (2000-2004) or follow-up survey (2013-2017). The survey included a self-report of sociodemographic characteristics and physical health conditions (Blood. 2010;116:3129-3) . The frailty phenotype was constructed from responses provided by BMT survivors using modified Fried criteria (JAMA Oncol. 2016;2:1277-86) . Details regarding cGvHD were abstracted from medical records. We conducted a systematic evaluation of the association between cGvHD and key chronic health conditions (xerostomia, dry eyes, cataract, glaucoma, diabetes, hypothyroidism, cardiomyopathy, coronary artery disease, stroke, tremors, problems with balance, pain, sensory loss, subsequent malignancies, esophageal or rectal/anal stricture, cirrhosis and pulmonary complications), using multivariable cox regression analyses adjusted for sociodemographics, primary diagnosis, smoking status, pre-existing comorbidities and TBI. We also examined the association between cGvHD and frailty using logistic regression and adjusting for the variables listed above, as well as chronic health conditions. Results: The 581 study participants underwent BMT at a median age of 30.9y (0.4-62.9) and participated in the study at a median age of 48.0y (18.2-73.7), after a median of 17.1y (2.0-40.5) from BMT; 55% were males and 77% were non-Hispanic whites. Primary diagnoses included CML (37%), AML (28%), ALL (14%), SAA (9%), other (12%). In this cohort of 581 allogeneic BMT recipients, 304 (52.3%) carried a history of cGvHD. All patients received myeloablative conditioning; TBI was used in 85%. The frequency of the following chronic health conditions was statistically-significantly higher in BMT patients with a history of cGvHD vs. those without cGvHD. (Fig 1): oral (difficulty in tasting/swallowing/chewing) and/or ocular (dry eyes) conditions (54% vs. 34%, p<0.0001), diabetes (17% vs. 11%, p=0.04), osteonecrosis (13% vs. 5%, p=0.002), neurological symptoms (tremors/decreased sense/prolonged pain: 33% vs. 23%, p=0.007), pulmonary complications (fibrosis/scarring/oxygen supplementation: 23% vs. 12%, p=0.0005), and GI complications (esophageal strictures + rectal/ anal strictures: 13% vs. 8%, p=0.05). The frequency of frailty was also higher in those with cGvHD vs. those without cGvHD (17.1% vs. 6.14%, p <0.0001). Overall, 45% of the allogeneic BMT recipients with cGvHD vs. 25% of those without cGvHD had 2 or more chronic health conditions (p<0.0001). As shown in Fig 1, multivariable analyses showed statistically significant associations between cGvHD and oral/ocular complications (HR=1.91, 95%CI, 1.4-2.5, p<0.0001), diabetes (HR=1.58, 95%CI, 0.96-2.6, p=0.07), osteonecrosis (HR=2.59, 95%CI, 1.4-5.0, p=0.004), neurological complications (HR=1.52, 95%CI, 1.1-2.2, p=0.02), pulmonary complications (HR=2.04, 95%CI, 1.3-3.2, p=0.002), and GI complications (HR=1.87, 95%CI, 1.1-3.3, p=0.03). In a multivariable model, adjusting for demographic and clinical variables and chronic health conditions, the odds of frailty were 2.66-fold higher among those with cGvHD (95%CI, 1.4-5.1, p=0.003) when compared with those without cGvHD. Conclusions: Allogeneic BMT recipients with a history of cGvHD carry a significantly higher burden of long-term morbidity, and are also at a significantly higher risk of frailty. The association between cGvHD and key chronic health conditions provides evidence for developing targeted surveillance and intervention strategies to reduce the burden of morbidity and frailty.
Arora: Takeda Oncology: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal